Chronic inflammation, a silent threat within our bodies, arises in response to various triggers like infections or injuries. Unlike acute inflammation, which is a quick and necessary defense mechanism, chronic inflammation can persist for a long time, quietly damaging tissues and organs. By understanding and addressing this hidden danger, we can work towards better health and well-being.
Distinguishing Between Acute and Chronic Inflammation
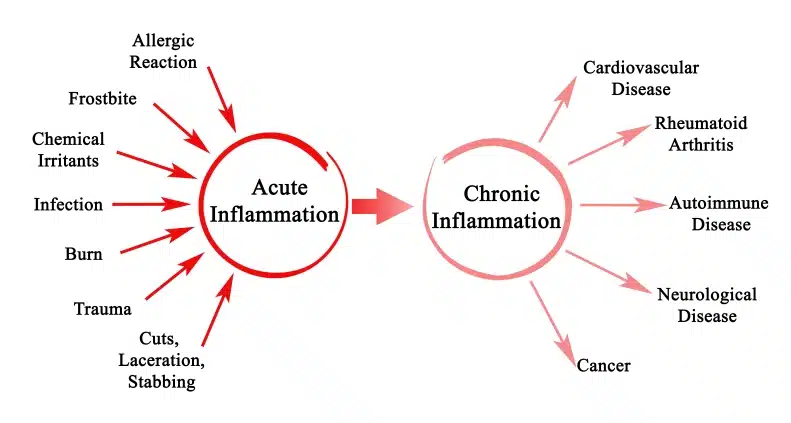
Acute inflammation is a fundamental biological response triggered by the body’s immune system in response to harmful stimuli, such as pathogens, tissue injury, or irritants. It is a rapid and short-lived response from the body that typically lasts a few days to a few weeks and is aimed at removing the source of damage and initiating tissue repair. It involves a well-coordinated immune reaction using chemical and immune cells in the body. Examples of acute inflammation include the body’s response to a cut or infection. Common signs of acute inflammation include redness, swelling, heat, pain, and loss of function at the affected site. While acute inflammation can develop things that are gross like pus and cause some collateral damage to your cells, it serves to protect the body. Once the threat is neutralized, inflammation resolves and tissue function is restored.

In contrast, chronic inflammation results in a dysregulated immune response that persists for weeks, months, or even years. Unlike acute inflammation, chronic inflammation can occur systemically and may involve multiple tissues or organ systems. It usually involves low-grade, persistent inflammation with subtle or no outward symptoms. Chronic inflammation can result from persistent exposure to irritants, such as environmental pollutants, chronic infections, autoimmune disorders, or lifestyle factors like poor diet, stress, and lack of exercise.
Understanding Chronic Inflammation
Understanding chronic inflammation is crucial because it plays a central role in the development of various diseases, including cardiovascular diseases, diabetes, cancer, neurodegenerative diseases, and autoimmune disorders. Unlike acute inflammation, which is a protective response, chronic inflammation can contribute to tissue damage, impaired function, and the development of chronic conditions. Moreover, chronic inflammation is intricately linked to aging and age-related diseases, highlighting its significance in promoting healthy aging and longevity.
Causes and Contributors
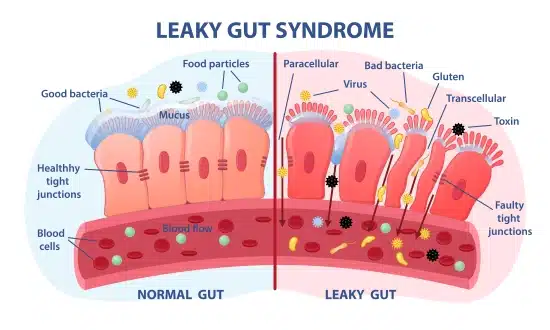
Chronic inflammation can be influenced by various lifestyle choices, including diet, stress, and sedentary behavior. Poor dietary habits, such as consuming high amounts of processed foods, saturated fats, and sugar, can promote inflammation. Delayed food allergies and leaky gut syndrome are also contributors. Chronic stress triggers the release of stress hormones, which can dysregulate the immune system and contribute to inflammation. Sedentary behavior and lack of physical activity have also been linked to low-grade systemic inflammation.
Exposure to environmental pollutants and toxins can contribute to chronic inflammation. Air pollution, cigarette smoke, heavy metals, pesticides, and industrial chemicals are examples of environmental factors that can induce inflammation by activating immune cells and generating oxidative stress. Chronic exposure to these pollutants can exacerbate inflammatory diseases and increase susceptibility to infections. Persistent or recurrent infections can also continuously stimulate the immune system.
Autoimmune diseases occur when the immune system mistakenly attacks healthy tissues, leading to chronic inflammation and tissue damage. Conditions such as rheumatoid arthritis, lupus, multiple sclerosis, and inflammatory bowel disease are characterized by dysregulated immune responses. Increased chronic inflammation can also make these issues worse.
Obesity and metabolic syndrome are associated with chronic low-grade inflammation. Adipose tissue produces chemicals that contribute to systemic inflammation and insulin resistance. Excessive calorie intake and imbalances in adipose tissue metabolism contribute to the development of obesity-related inflammation and metabolic dysfunction. Additionally, metabolic syndrome, characterized by abdominal obesity, dyslipidemia, hypertension, and insulin resistance, further exacerbates inflammation and increases the risk of cardiovascular disease and type 2 diabetes.
Health Implications of Chronic Inflammation
Chronic inflammation can affect multiple organ systems in the body, leading to a range of health issues. In the cardiovascular system, inflammation contributes to the development of atherosclerosis and plaque formation, increasing the risk of heart attacks and strokes. In the digestive system, inflammation is associated with conditions like inflammatory bowel disease (IBD), gastritis, and peptic ulcers. In the nervous system, it plays a role in neurodegenerative diseases like Alzheimer’s and Parkinson’s, as well as in conditions like multiple sclerosis. It is also reported to affect other problematic diseases like diabetes (type 2 diabetes and insulin resistance) and cancer (various types including colorectal, lung, and breast cancer).

Ever notice that other people your age might appear significantly older or younger than you do? Chronic inflammation is considered a hallmark of aging and is implicated in the progression of age-related diseases. As individuals age, the immune system changes, leading to increased production of pro-inflammatory chemicals. This chronic low-grade inflammation contributes to the development of age-related conditions such as cardiovascular disease, neurodegenerative diseases, frailty, and functional decline.



Emerging evidence suggests that chronic inflammation may contribute to mental health disorders such as depression, anxiety, and cognitive decline. Inflammatory markers have been found to be elevated in individuals with mood disorders, and chronic inflammation may disrupt neurotransmitter function, neuroplasticity, and neurogenesis in the brain. Additionally, it is associated with increased oxidative stress and damage to brain cells, contributing to cognitive decline and the development of neurodegenerative diseases like Alzheimer’s. This means that managing inflammation might have implications for improving mental health and cognitive function.
Managing Chronic Inflammation
Adopting an anti-inflammatory diet rich in whole foods, such as fruits, vegetables, and healthy fats, can help reduce inflammation. Foods high in omega-3 fatty acids, such as fatty fish, flaxseeds, and walnuts, have anti-inflammatory properties. Additionally, consuming foods rich in antioxidants, such as berries, green leafy vegetables, and nuts, can help neutralize free radicals and reduce inflammation.

Managing stress through techniques like mindfulness meditation, deep breathing exercises, and yoga can help reduce inflammation and promote overall well-being. Regular exercise has anti-inflammatory effects and can improve immune function and cardiovascular health. Prioritizing adequate sleep is also essential, as insufficient sleep can increase inflammation and negatively impact immune regulation.
Complementary and alternative therapies, such as meditation, and herbal remedies, may help reduce inflammation and promote healing. Mindfulness meditation and relaxation techniques can help lower stress levels and reduce inflammation. Certain herbs and supplements, such as turmeric, ginger, and green tea, have anti-inflammatory properties and may complement conventional treatments for managing chronic inflammation.

Chronic inflammation is not just a passive bystander in the development of various diseases but rather a driving force behind their formation. It serves as a common denominator linking diverse conditions such as cardiovascular diseases, diabetes, cancer, and neurodegenerative disorders. Understanding the underlying mechanisms and contributors to chronic inflammation provides valuable insights into disease prevention, diagnosis, and treatment. Recognizing the systemic impact of chronic inflammation underscores its significance as a target for therapeutic intervention and highlights the need for proactive management strategies.
Conclusion
Given the pervasive role of chronic inflammation in promoting disease and accelerating aging processes, there is an urgent need to prioritize inflammation management as a cornerstone of preventive healthcare. Individuals can take proactive steps to mitigate chronic inflammation by adopting healthy lifestyle habits, including a balanced diet rich in anti-inflammatory foods, regular exercise, stress management techniques, and adequate sleep. These steps can enhance their quality of life and promote longevity.
Healthcare providers should play a crucial role in educating patients about the impact of chronic inflammation on health outcomes and guiding them toward evidence-based interventions to mitigate inflammation and improve overall well-being. The problem is that most healthcare providers receive almost no training in nutrition, leaving them ill-equipped to address the role of diet in managing chronic inflammation and promoting overall health. Additionally, the current healthcare system prioritizes quick visits and writing prescriptions over lifestyle interventions, providing little incentive for physicians to prioritize nutrition education and counseling. As a result, patients rarely receive adequate guidance on dietary strategies to mitigate inflammation and improve their well-being, highlighting the need for a shift towards comprehensive, patient-centered care that encompasses nutrition education and lifestyle interventions.
The field of inflammation research continues to evolve rapidly, uncovering novel insights into the intricate mechanisms underlying chronic inflammation and its role in disease pathogenesis. Ongoing efforts focus on identifying biomarkers for early detection and monitoring of chronic inflammation, elucidating the interplay between genetic, environmental, and lifestyle factors in inflammation regulation, and developing targeted therapies to modulate inflammatory pathways. Collaborative interdisciplinary research efforts are essential for advancing our understanding of chronic inflammation and translating scientific discoveries into innovative strategies for disease prevention and treatment. By embracing a proactive and integrative approach to inflammation management, we can pave the way toward a healthier and more resilient future.
